We began fundraising for congenital heart defect (CHD) research the moment Graeme was born in 2012. That was when we first learned about congenital heart defects (CHDs). Nine years later, we started our own non-profit in his name, The Graeme McDaniel Foundation.
Our mission is to fund congenital heart defect research and support heart families.
The Graeme McDaniel Foundation is excited to grow and strengthen relationships with heart centers around the country. We are learning of these centers’ planned research projects and hearing how additional support from our foundation can progress their hard work. We will be able to choose which projects we support with the money you help us raise, and we are excited to share the progress and outcomes of these projects. Please fill out our inquiry form to be considered for future grant funding from The Graeme McDaniel Foundation.
Congenital Heart Defect Grant Awards
Cellular Signaling and Stem Cell Therapy in Congenital Heart Disease
The proposed research plan will provide critical data related to the underlying inflammatory signaling mechanisms and downstream cellular effects that promote the deleterious development of endocardial fibroelastosis (EFE) and scarring in the developing heart. A new in vitro model of EFE will serve as a novel experimental platform to support the development of future treatment and therapeutic options for affected babies. The primary goal is to investigate cellular mechanisms to identify progenitor cell (stem cell) - based therapies to combat scarring of the inner surface of the heart that leads to abnormal functioning and development of the heart in congenital heart disease.
As lead scientist, Dr. Damien J. LaPar MD, MSc states, “We believe that by understanding the underlying mechanisms, we are going to be able to develop cellular and regenerative therapies either through stem cells or pure cellular-level signaling cascades that could arrest that process, [then] reprogram those scar-forming cells so they can form [healthy heart] muscle.”
The Graeme McDaniel Research Scholar
The Graeme McDaniel Research Scholar will be awarded to one of Texas Children’s Hospital’s faculty over a period of one year to support their work in preparation for future applications for ongoing congenital heart defect research funding. Through this mechanism, the fund will achieve significant financial leverage through its support of bright early-career researchers enhancing their ability to obtain career-defining long-term research funding. The potential to follow these advanced individuals and maintain relations with them as they grow in their career is invaluable. With a 3-year commitment, we look forward to funding three Graeme McDaniel Research Scholars.
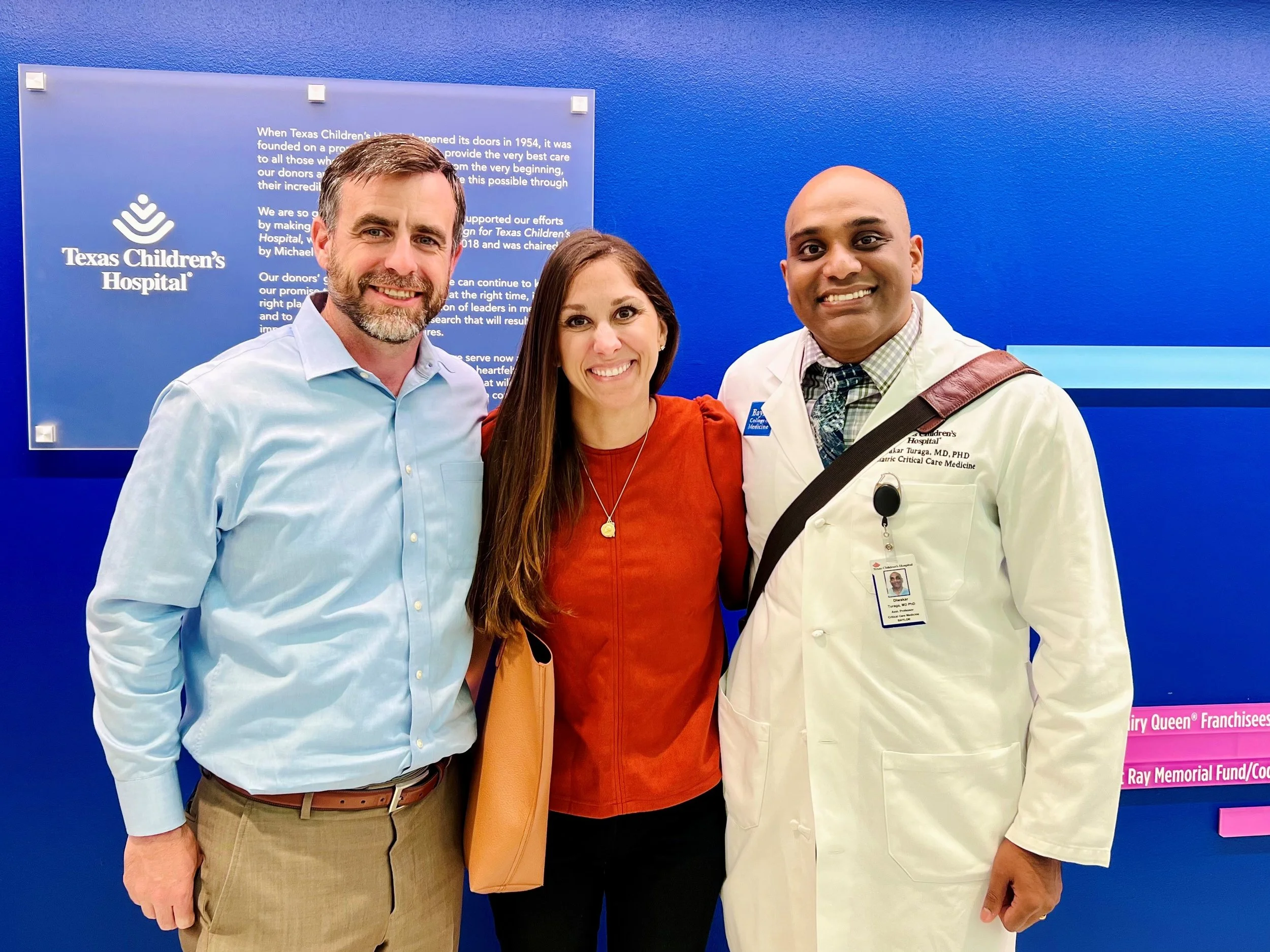
year 1 (2022-2023) -
"Complex congenital heart disease (CHD) patients invariably require complicated surgical repairs. Despite the best possible surgical repair, some of the patients develop heart failure. My research is focused on applying cutting edge genomic tools to understand why the heart muscle fails in these patients. The CHD heart muscle faces abnormally high amounts of stress and works tirelessly, and our recent results show that the CHD heart muscle ages faster than expected. Now that we have an insight into why these CHD hearts fail, we can start working on making the heart muscle stronger [by using precision medicine]." Dr. Turaga
You can read more about Dr. Turaga’s work in his Nature paper and in this interview.
Update on 2023 projects: In certain serious conditions like congenital heart disease, the RV may pump blood into the body instead of just to the lungs. In very rare cases, some people have what's called a 'super RV', where these stressed RVs continue to function well even into later stages of life. In this study, we looked at the genetic activity of ‘super RV’ from a 60-year-old person who had a specific type of congenital heart defect called congenitally corrected transposition of the great arteries (ccTGA). We found that in this person's RV, there were two important pathways that were more active than usual, a pathway related to insulin-like growth factor (IGF1) was more active and increased activity in pathways related to the growth of new blood vessels (angiogenesis). These findings suggest that in rare cases, the RV might last much longer by adapting to the extra strain by becoming more responsive to growth signals and by growing new blood vessels. Understanding how the RV adapts to increased stress is important for developing better treatments for congenital heart disease. Now that we know 'WHAT' genes to target, next steps will be 'HOW' to target the genes in the heart. We can potentially repurpose existing drugs which target these pathways (used for cancer, endocrine diseases) to treat RV failure or use gene therapies to specifically treat heart cells. Both approaches are promising, now that we know 'WHAT' to target. The detailed paper can be found here.
Diwakar Turaga, MD, PhD Assistant Professor of Pediatrics, Section of Critical Care Medicine, Baylor College of Medicine
year 2 (2023-2024) -
We are honored to announce Tam T. Doan, MD, MS, RDCS as our 2nd year Graeme McDaniel Research Scholar! We cannot wait to share more soon.
The team at Boston Children's Hospital has created a program that uses imaging to create computational fluid dynamics (CFD) models of patients’ hearts. With these models, the team can offer much greater care to children that require surgical interventions. The models enable surgeons to simulate surgical repairs. In addition to having a much better idea of the patient’s specific anatomy before conducting the surgery, the team can use these modeled repairs to see how flowrates and pressures in the heart will react to the planned surgery. Another important use for these models is to give a much more detailed measurement for cutting 2D patches that surgeons will install into a 3D heart. Without the model, the surgeon is often making corrections to the patch during the actual surgery. The model can also be used to simulate how any surgical repair will react as the child continues to grow. With the money from The Graeme McDaniel Foundation, the team at Boston Children's Hospital will be able to hire additional engineers to expand the program and service more children. The ultimate goal is to roll this process out to major heart hospitals all across the country. This video focuses on the collaboration between engineers and surgeons, and the tremendous impact their work has had on so many families.
2023 Update “Support from the Graeme McDaniel Foundation has been critically important as we extend our clinical 3D modeling program into computationally planning patches for repairs inside the heart and can take those plans into the operating room for the surgeon to use as a guide to determine the shape and size of the patch. This is a very exciting advancement to improve the geometric and clinical outcomes of some of our most complex repairs.” Dr. Hoganson
A large percentage of CHD patients require valve replacements. The good news is that valve repairs have improved greatly over the years. The bad news is that there isn’t a good source of artificial valves for doctors to use on young children. Typically, the goal is to give the child enough time to grow large enough that the smallest available adult valve can be used. The problem is that these valves are still typically too large, and they can cause issues that require additional intervention. PolyVascular is a company founded by doctors with the goal of developing artificial valves that are sized specifically for small children. Because the market for adult valves is so much larger than valves for young children, these children’s valves have never been able to attract enough funding to get a product from design all the way to market. By raising money from The Graeme McDaniel foundation and others, PolyVascular will develop a valve that is specifically designed for small children. They will pair the valve with a delivery system that will allow the valve to be placed by catheter instead of open-heart surgery. Hospital time will be greatly reduced and future complications from a poorly sized valve will be eliminated.
2023 Update In the six months since receiving funding from The Graeme McDaniel Foundation and other supporters, PolyVascular has made significant strides in advancing their mission to develop artificial pulmonary valves tailored for small children with congenital heart defects. The Graeme McDaniel investment has helped fuel extensive valve testing and the beginning of a robust pre-clinical study.
Valve testing includes ensuring the deliverability, performance, and durability of the valve design. Valve testing is a rigorous process starting with the careful manufacturing and inspection of the valve. These benchmark tests help PolyVascular to ensure the highest quality standards are met for their valves. Testing over this time showed favorable results, exciting the team as they moved into the pre-clinical study.
The 90-day pre-clinical study began at the end of 2023 and is ongoing. Initial results from the study yielded remarkable achievements in performance and durability.
The valve testing and pre-clinical study mark two very significant achievements for the team. These two milestones were met due to the amazing support of our investors including the Graeme McDaniel Foundation. PolyVascular is excited to continue their work in 2024 and report further success!